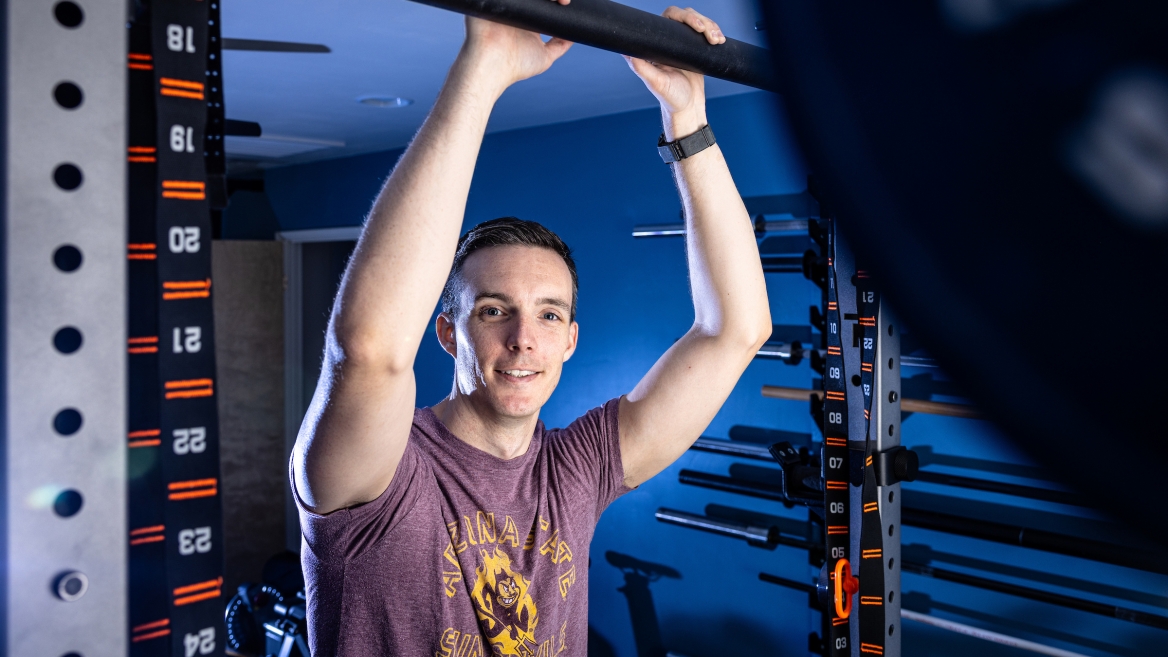
New nursing professor connects body and mind in life, research
By
—
Editor's note: New Faces on Campus is a new monthly feature by ASU News showcasing faculty members who have been hired in the 2022–23 academic year.
Zachary Baker believes in order to keep a sharp mind, the body must follow suit.
Every day he works out for at least an hour, alternating between the rower, the stationary bike, floor exercises and a weightlifting regimen.
“I've been working out pretty consistently since my second or third year of grad school,” said Baker, who is a new assistant professor in the Edson College of Nursing and Health Innovation at Arizona State University. “Universities easily have the best gyms for the price.”
But when the pandemic hit, Baker built his own home gym. He continues to work out because he knows the mental lifting he does at ASU will require all his physical strength.
Baker’s research focuses on understanding former caregivers of people with dementia so he can help them garner the psychosocial resources and technological tools to thrive. A methodologically uninhibited researcher, Baker enjoys digging into complex quantitative data, nuanced qualitative data and rich theory alike.
ASU News spoke to Baker about his work, his workouts and why he is drawn to his research.
Editor's note: Answers have been edited for length and clarity.
Question: Can you tell us a bit about your background — where you’re from and how you ended up in academia?
Answer: Born and raised in the suburbs of Philadelphia. To get to my hometown, go down the Main Line and stop just before you hit the Amish farms. If you hit them, you’ve gone too far. If they’re not yet in sight, you haven’t gone far enough.
I got to where I am mostly through a lot of serendipity and several mentors who were willing to take a chance on a fairly inquisitive and incredibly ignorant kid. In high school I was more interested in making jokes than schoolwork. Once I got to college, I had a pretty serious about-face because I knew my mom was paying a lot of money for it on her own and I didn’t want to waste that. I planned to be a lawyer, took all the political science classes my school offered, and planned to transfer to a higher-ranked institution to give myself the best chances of getting into a good law school. A quirk in the scheduling meant I had an extra semester where I didn’t know what to take so my mom told me to take a psychology course. I thought that was a waste of time, but I had time to waste. That semester I switched; became a psych major with almost no idea what one does with a psych major.
Went to grad school for social psych, ... spent a lot of time studying how to live our best lives and determined that one of the most important things was to do something that mattered. I had some protected time due to a bit of luck with some grants and decided dementia was a place where I could apply the things I learned, so I did a postdoctoral learning about dementia care. ... I spent that time figuring out what I could do in dementia care that wouldn’t get done if I didn’t do it. I realized that this was working to improve the lives of former caregivers of people with dementia — i.e., those who are bereaved.
Q: What is your area of research or academic focus? What are you most excited about regarding your work?
A: My work is all about trying to understand former dementia caregivers so I can help improve their lives. The vast majority of folks who used to care for someone with dementia do just fine. They grieve and move forward after some time. But here’s the thing: Almost everyone has some sort of personal connection to dementia. I know this because when I tell people what I do they almost always have a story to share. I also know this because upper estimates suggest that around 1 million people became newly bereaved after caring for a person with dementia last year in the United States. When you’re dealing with these kinds of numbers, even a small proportion of folks suffering is a lot of folks. Right now, our best guesses suggest that around 250,000 of these million each year suffer from a grief so great that it meets the criteria for a clinical disorder.
When I think about what excites me the most about my work, it’s the fact that I might be able to move the needle on how to help people. I’m incredibly lucky that hundreds of former dementia caregivers have given me their time to teach me about their lives. These are the people who I think about when I write a new article or run a new statistical test. It’s not some ethereal former caregiver, … it’s Warren or it’s Sheryl.
Q: When did you realize you wanted to study this field? What was your “aha” moment?
A: I knew I wanted to focus on former dementia caregivers when I started attending a group of former caregivers in December 2019. I’ve gone to every meeting they’ve had, with two to three exceptions, since. It’s a group of former caregivers who help each other figure out what’s next.
This group’s mission is so vital because, of the hundreds of former dementia caregivers I’ve talked to, two things come up almost every time: “Who am I?” and “Where do I fit in?” If you yourself are a former dementia caregiver, you might know exactly what I’m talking about. If not, here’s a story I think about every day that might help.
Sheryl was a corporate IT project leader who was helping our nation's corporations work through uproarious things like Y2K. She took a couple months off to help her mom recover from heart surgery and those months turned into 12 years, in which she took care of both her parents and both of her husband's parents. Two of those parents developed dementia and then, in just over a year, all four died. Sheryl had gone from an important corporate job, to an important job caring for four of the most important people in her life, to ... what? As she once put it to me, she wasn’t going back to IT — 12 years made her a dinosaur in that world. And there was no longer anyone who needed her care. Sheryl was left in the lurch. She had been great at both jobs.
My “aha moment” comes most days when I hear from one of the millions like Sheryl.
Q: How do you want to see this field advance to the betterment of society?
A: When I look back on my career, I want to say that no former dementia caregiver is left in the lurch. Ideally, I can help stop anyone from ever struggling in the first place. Absent that, I at least want people to know where they can turn for help. I want everyone to have a place to go to find resources to answer those two questions I mentioned: "Who am I? Where do I fit in?"
I also spend a lot of time trying to convince other researchers to join the field. I have a handful of other colleagues thinking about and working to improve the lives of former dementia caregivers. I have thousands working on the time when a person with dementia is still alive. And the population I serve grows by a million each year.
Q: What is something you wish more people realized about your work or research?
A: It takes about 17 years for an intervention that works to hit real people. That’s just too long. And that’s for the tiny proportion of interventions that work. We need to think in different ways and explore different avenues to getting our work to real people. Getting effective interventions to people taking almost the same amount of time as raising a newborn into a legal adult is not something I can abide.
Q: What brought you to ASU, and what do you like about the university?
A: The things Edson College and ASU wanted were the things I was already planning to do. To hit the scale I want in my research, I need grants. To have the kind of impact that transcends what one person can do with a career, I need to teach. To get out of bed every day for 40 years reaching for the same pie-in-the-sky goal, I need to engage with people in the community.
Q: What’s something you do for fun or something only your closest friends know about you?
A: I got involved in building a home gym while we were all locked down during COVID. Somewhat ironically, that led to making friends all over the world talking about home gyms. We’ve even done a bunch of online powerlifting competitions. Though I should acknowledge, it’s not just my closest friends who know. I try to talk about my home gym with anyone who will listen.
Top photo: Edson College of Nursing and Health Innovation Assistant Professor Zachary Baker focuses his research on understanding, developing, evaluating and disseminating technological tools to help caregivers and persons with dementia thrive during and after the caregiving process. He works out to relax and stay sharp. Photo by Charlie Leight/ASU News
